By nat levy
I slip my fingers through a pair of metallic rings; my eyes go to a viewfinder-like set of cameras and my foot compresses a pedal. From the outside, this might sound like playing flight simulator or a virtual driving game, but what I’m actually doing is operating a da Vinci surgical robot. There are only about 5,500 of these machines in the world, and they cost about $2 million apiece.
Once I’m settled in, I have a simple task: control a pair of robotic arms with needle-nose plier-like hands to pull a tiny pin out of faux human tissue and then reinsert it. Think about the childhood game of Operation, but add a multi-million-dollar piece of cutting-edge medical equipment and the challenging nature of the faux tissue, and you’ll get a good mental picture.
I was able to slowly and delicately pick up the pin, but replacing it was another deal entirely. I was afraid of applying too much force and damaging the tissue. I accidentally dropped the pin, and in contorting the arm to try to pick it up again I failed the experiment. The arm locked up because I put too much torque on it. Essentially, I broke the robotic wrist.
Da Vinci machines have completed more than 7 million surgeries around the world, and that number is growing rapidly. The University of Texas at Austin is one of only a handful of institutions in the country with more than one da Vinci surgical robotic system to experiment on.
It’s a sign of strength for UT in an emerging field known as SURGINEERING.
What is Surgineering?
The word itself is the combination of surgery and engineering, which is also an adequate definition of the concept. At the most basic level, surgineering is a new field of research that sees engineers working closely with surgeons to solve problems in the operating room. This could be through new tools and devices, better ways to use existing technology and new ways to prepare surgeons before they ever work on a human patient.
The core aspects of surgineering, such as medical device manufacturing and biomedical engineering have been around for a long time. But what’s different is these areas coming together to examine pain points for patients and surgeons and solve them not just with medical skill but with engineering tools and concepts.
The partnerships between surgeons and engineers are the key ingredient of surgineering. Surgeons know what the need is in the operating room but may not have the technical abilities to create a solution. And engineers may have great ideas for improving surgical tools, but they don’t have a chance to see the problems firsthand.
Additionally, the lack of pipeline between the two fields made it challenging to come together and collaborate.
Everything was siloed,
said Dell Med Division Chief of Minimally Invasive Surgery John Uecker. The clinicians didn’t know how to get to engineers, and engineers didn’t know how to get to clinicians.
Uecker co-founded a startup called ClearCam with Texas Engineer Chris Rylander and other Cockrell School researchers. He is a major proponent of surgineering team-ups.
The term itself is used rarely — several of the experts interviewed for this story don’t even use it. Jeff Siewerdsen, vice chair for clinical and industry translation in the Department of Biomedical Engineering at Johns Hopkins University, is thought to be the originator of the term. But it is starting to spread to other institutions, as researchers see the value in collaborations between surgeons and engineers.
The concept remains so new that there isn’t even consensus on the best way to spell it.
We asked everyone we talked to for this story, three engineers and four surgeons, how they would spell the word. And by a slim margin, surgineering
won out over the alternative spelling of surgeoneering.
Some engineers and clinicians freely use the term; others say it’s not a thing yet. But it’s clear that collaborations between surgeons and engineers are on the rise. These alliances will result in a more robust technical toolkit in the operating room to make life easier for surgeons and improve patient outcomes.
“Engineers speak their engineering language, and surgeons speak their surgical language. There’s an opportunity to create a new field that bridges this gap, and it just needs a critical mass of individuals on both sides to cross over and learn how to speak their colleagues’ language.”
-Ann Majewicz Fey, a professor in the Cockrell School of Engineering’s Walker Department of Mechanical Engineering
UT Austin is among the places most well-equipped to become a leader in this new field. The Dell Medical School is a big part of its potential. At only seven years old, it is the first medical school in nearly 50 years to be built from the ground up at a top-tier Association of American Universities research university.
This young and nimble medical school, a top 10 engineering institution in the Cockrell School and a culture of innovation in the surrounding area represent a potent combination with the potential to hatch new ideas, get them built and out into the market.
UT Austin has the foundation of a great surgineering ecosystem being built from the ground up,
said Jordan Amadio, a neurosurgeon at the Seton Brain & Spine Institute and an affiliate faculty member at Dell Med. And we have a chance to attract like-minded surgeons and engineers who will continue to grow the ecosystem.
We talked to several engineers and surgeons for this story, and while these collaborations are becoming more common, it’s clear that surgineering remains a nascent field. And we’re only starting to scratch the surface of what engineers and surgeons can accomplish together to save patient lives and improve their experiences.
Bridging the Experience Gap
Despite massive advances in medical technology, surgeons generally learn the same way they have for generations. Despite technology advances, the fact remains that the best way to become a surgical mastermind is to do a lot of surgeries.
One pillar of surgineering is finding new ways to train surgeons that can make up for an experience gap when compared to more seasoned surgeons. No one wants to be the first person to be operated on by a surgeon.
Kimberly Brown is a surgical oncologist and educator at Dell Medical School. She notes that learners and trainees have typically been taught under what she calls the see one, do one, teach one
method. That is, they observe experienced surgeons perform procedures, then they join surgeons in the operating room to assist, before eventually performing the surgeries themselves.
This method, Brown says, goes against what we now know about education, especially when it comes to teaching technical skills.
You wouldn’t put a baseball player on the mound and say ‘watch me pitch, now you pitch a couple times, now go play professional baseball,’
Brown said.
Giving aspiring surgeons more ways to sharpen their skills before ever operating on a patient is a focal point of Fey’s research. Fey also has a courtesy appointment as an associate professor at Dell Med’s Department of Surgery and Perioperative Care. Before joining UT Austin last year, she spent six years at UT Dallas, and she brought a da Vinci system with her to the Forty Acres.
Fey and her students are working on several projects creating educational tools for surgery. Many of these projects use haptic feedback, which involves vibrations and other sensations that give the user a sense of touch.
One example focuses on the trocar, a pen-shaped instrument used in laparoscopic procedures that includes a sharp point and hollow tube to provide a path for devices to follow during surgery. Installing a trocar is often the first step in a surgery, and a place where mistakes can happen. Less experienced surgeons, Fey says, may push the device too far into the body and potentially damage organs.
Any errors in a patient can be catastrophic, so it’s extremely high stakes,
Fey said. People expect excellence in their surgeons, so the more we can develop technology to speed up that learning curve and achieve higher levels of mastery, the more we can one day improve patient care.

Ann Majewicz Fey and her researchers work with a haptic glove that gives feedback to the user on the amount of pressure being applied.
Fey and her team are working on a way to practice placing trocars using a haptic simulator that allows users to feel tissue resistance and understand how hard they have to push to deploy the trocar. And there are ways to modify the haptic feedback of the device for all different types of patients, each of whom require a different level of force to get the trocar into the body.
This project fits into a broader theme that surgeons noticed amongst their trainees: they use too much force with their instruments. Another one of Fey’s projects aims to curb this issue. The researchers created a constraint device that attaches to basic surgical tools, that includes a piece of soft silicone. As the user’s grip tightens, the device pushes back to let the surgeon know they are holding on too tight.
When you over-grip surgical instruments, it’s easy to damage sensitive tissue, and that’s something we want to mitigate,
Fey said.
Fey’s team works out of the renovated Anna Hiss Gym, where Texas Robotics is housed. The creaky wood floorboards and old basketball hoops provide an interesting contrast with the cutting-edge research happening within the bricked-wall space where natural light cascades in.
Fey’s team is using their da Vinci for interesting training purposes. The team just submitted a new paper analyzing calm versus anxious movements in surgeons using the robot for training.
Fluid movements are critical in surgery, and mapping surgeons’ movements could be an easy way to help them improve their performance. The goal is to provide guidance forces
that help them learn how to better control their movements in the ultra-tight space of a surgery.
In the experiment we turned on different types of haptic guidance cues whenever the user’s movements started to have this anxious signature, and we actually had significant results that we were able to improve their style,
Fey said.
Robots in the Operating Room
While robots play a significant part of Fey’s surgical training research, they’re also becoming more common in operating rooms. An analysis of procedures performed on 170,000 patients at 73 hospitals published last year showed that robots were involved in more than 15% of surgeries in 2018, up from just shy of 2% in 2012.
And it tracks with how new surgeons are trained nowadays. Abigail Cain just finished her obstetrician-gynecologist residency, and she is beginning a minimally invasive gynecological surgery fellowship at Dell Med. That involves two years of training in robotic and laparoscopic surgery for endometriosis and tumors in the uterus called fibroids.
Cain, who has worked with Fey on some of her projects, noted that most of her fellow residents came out of the program certified to work with robots. Using robots during surgery leads to fewer instances of open procedures
meaning keeping incisions small rather than having to open up the patient. Open procedures are more dangerous for patients and increase the odds of complications.
Plus, robots reduce the physical toll on surgeons, who typically have to stand in place for hours for most procedures and perform painstaking, precise movements the entire time.
Working with robots is a lot less physically demanding,
Cain said. And they have more flexibility than we do, so they can navigate around areas where there isn’t a lot of room.
Robotics in the operating room and new devices to enable better procedures are at the core of Farshid Alambeigi’s work. He joined UT Austin in 2019, coming from Johns Hopkins University, and he runs the Advanced Robotic Technologies for Surgery Lab in the Cockrell School. He also appears to be one of the originators of the term surgineering.
Surgineering bridges the gap between surgeons and engineers to develop technologies for elevating surgeons’ skills to further improve quality of the surgery together with patients’ safety and quality of treatment.-Farshid Alambeigi, an assistant professor in the Walker Department of Mechanical Engineering
Like Fey, Alambeigi is in possession of a full da Vinci robot, the one I tried to handle the pin with and failed. They are working on ways to use the robot as something of a surgical assistant, that can provide an extra arm to do tasks like stretching tissue to make it easier for surgeons to cut it. And they want to make it possible for this to happen autonomously.

One of the da Vinci surgical robots that the engineering teams use for practice and testing.
These robots can be used by surgeons for minimally invasive surgeries. The thinner, smaller arms of the da Vinci are much easier to get into the human body than the hands of a surgeon, speeding up patient recovery times.
If you don’t have to open up the patient to allow all these hands to come in, and instead you just have to make two holes, it’s better for the patient because it allows them to recover way faster,
said Manuel Retana, a surgical robotics Ph.D. student in Alambeigi’s lab, who has also worked on robotics projects at NASA. This has not always been the mentality in the medical field in that they always did surgeries a certain way, but this really allows you to re-think how you go about approaching surgeries.
The researchers are even working on the ability to operate these machines remotely. That would allow, for example, a surgeon in the top of the field located in Italy to perform a procedure remotely on someone at a hospital in Houston.
Alambeigi and his team are also developing bendable screws and a steerable robotic drill that can give surgeons the ability to chart new, curved trajectories through the body for procedures like spinal fusions, where vertebrae are fused together for different purposes such as bone recovery and to relieve back pain.
Today, because of the rigidity of surgical tools, the path for inserting screws must be a straight line, which means the screws may not be able to reach the best spots for connecting vertebrae. The process of placing these screws is long and labor intensive, and the number of X-rays required can lead to significant radiation exposure.
With these curved trajectories, we can anchor the implant in a place where there’s more bone density, which reduces the risk of failure, and we expose the patient to less radiation as well,
Alambeigi said.
The desire to decrease radiation, while still getting a clear image of what’s happening during the procedure inspired another of the team’s projects, an ultra-thin optical microfiber sensing system. It looks like a copper wire, and it is just 20 microns in diameter (or approximately one to two human hairs) and can be embedded in a number of devices. This optical fiber takes accurate measurements of force and shape of flexible instruments in the body, which is important during surgery where the margin for error is nearly zero.
The team’s ultra-thin optical microfiber sensing system, which takes accurate measurements of force and shape of instruments in the body.
Alambeigi works closely with Jordan Amadio, the Dell Med neurosurgeon. Their main project together is spinal fusion using flexible implants and curved drilling technology, but there are others as well.
Amadio, who also has an MBA from Harvard University, sees a massive commercial industry forming around surgineering and surgical robotics. In the 10 years he has been out of medical school, he said, technology has exploded in the field. And he is very passionate on what the next 10 years will bring in areas like artificial intelligence and machine learning and especially robotics.
“Over the next 10 years, robots will become ubiquitous and essential in all fields because they can act as an extension of what the surgeon can do,” he said. “They do not replace the surgeon; instead, they allow us to do things we couldn’t without the robot.”
Patient-specific Game Plan
There are two core areas of surgineering – creating new tools and technologies to improve surgery and finding better ways to use existing surgical tools. As part of the latter, engineers are using computer simulations to show how patients may react to procedures a week, or a month, or six months down the line.
As the cliché goes, no two people are the same. That certainly holds true when thinking about medicine and the human body. And when you’re talking about the high stakes of surgery, it’s important to understand that people may have incredibly different results after receiving the same procedure.
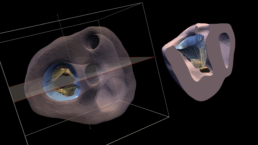
This conundrum is the basis for much of Michael Sacks’ work at UT Austin. He is a professor of biomedical engineering in the Cockrell School and the director of the Oden Institute’s Willerson Center for Cardiovascular Modeling and Simulation. His work falls under the wider umbrella of computational medicine.
His focus is on developing patient-specific, simulation-based approaches for treating heart and valvular diseases. Sacks and his research team use clinically obtained information from patients, especially the geometry of the heart, to simulate how it will react to a particular procedure and what the outcome could be six months to a year later.
The problem is that surgeons, when deciding the best treatment options, do not always have sufficient information to understand what’s happening with each individual patient,
Sacks said.
One area of the team’s research is mitral valve regurgitation, a condition where the heart’s mitral valve doesn’t properly close, allowing blood to flow backward. There are now promising, minimally invasive procedures that aim to clip the leaflets of the valve, allowing them to close properly. While successful in some patients, others do not fare as well and often have to undergo repeated procedures.
To address this issue, Sacks and his team are working on an ongoing project to simulate outcomes of the clipping procedure using pre-treatment clinically obtained imaging. To date, they’ve found that they can predict with 83% accuracy how the patient will respond to surgery six months in the future.
This work really underscores the need to look at this procedure in a patient-specific manner because the geometry and the physiology of each patient seems to have quite a notable impact on how well this treatment works,
said Natalie Simonian, a graduate research assistant in Sacks’ center.
Breaking Down Barriers
Engineering and surgery are very different fields, but the people drawn to them share similar mindsets. They’re fixers, builders. They are always looking for new ways to do things. However, sometimes — both surgeons and engineers say — they can fall into the trap of creating a solution that doesn’t necessarily address a known problem.
As engineers, we can be notorious for creating a hammer that’s looking for a nail,
Fey said. We like to design new things and develop new things, but making sure our designs are rooted in understanding what the user truly needs will help make sure that what we create is relevant and useful.
This is why collaboration is a cornerstone of surgineering. The engineers don’t know what the surgeons need; and the surgeons don’t know what the engineers can do. By building these bonds between the two disciplines these groups can build tools that help surgeons do their jobs better and in turn lead to better patient outcomes.
“Engineers alone and surgeons alone often don’t come up with ideas that are workable,” Amadio said. “It’s only when they get together that magic happens.”
And we are already seeing examples of this increased collaboration. There are courses that bring students from engineering disciplines like biomedical engineering into operating rooms early in their studies, planting the seeds for future surgineering collaborations. Both the surgeons and the engineers mentioned new groups and events that have started in recent years to emphasize collaboration between them. And recently, UT inked a partnership with the MD Anderson Cancer Center that will see several Texas Engineers, including Alambeigi, working on innovative projects to end cancer.
John Uecker has seen the rise of surgineering at UT Austin from all angles. He is the division chief of minimally invasive surgery at Dell Med and an executive at a UT Austin spinout company called ClearCam, which was developed with mechanical engineering professor Chris Rylander and which Alambeigi also works with. This company, very much a surgineering startup, and brought to fruition through Dell Med’s Texas Health Catalyst, makes a device that can clean the lens of a laparoscope while it’s in the body. This eliminates the need to pull the scope out of the body and speeds up procedures. It makes life easier for surgeons who often have to perform surgeries with sub-optimal vision due to dirty scopes.
The rise of Dell Med,
Uecker says, has accelerated the destruction of silos that previously separated engineers and clinicians. With these walls beginning to crumble, a pipeline between surgery and engineering is forming.
Uecker says he is excited by the way these collaborations have created a hub of innovation, surrounded by Austin’s growing startup scene that is chomping at the bit to commercialize these discoveries.
There’s still a lot of room for improvement,
Uecker said. With the development of this innovation district that is germinating in Austin and around surgineering in general, there is huge potential. I think we are just getting started.






